Everything about my infusion last Monday, July 7th, went
smoothly. I saw the PA, and we discussed
my two concerns. One, my acid reflux is back full force. It really can make my
days miserable. She said I could up the dose of the current over-the-counter
remedy that I have been taking. The statistics show that 9% of patients on TDM1
experience reflux. Since I have had this in the past, I can't say for sure my
treatment is causing this, but I did not have this problem with the other
treatment. On the 25th, I have an appointment with a gastroenterologist.
Hopefully, he will be able to prescribe something to help relieve it. Second, I
had her check two little red spots on my neck and one on my chest. Those spots
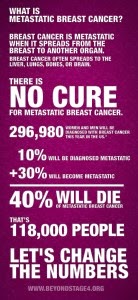
were worrying me because, believe it or not, breast cancer can metastasize to
the skin. The more I read the more I find this disease has no boundaries. The
verdict for the red spots was not cancer, whew! What they are is still unclear.
For now I am not going to worry about them.
On Thursday, I met a new oncologist. This doctor was to be a new
member of my team, one that would be able to order the drugs necessary for my
treatments in Wilmington. While speaking with him, I asked how often he does
brain scans. His answer made me remember my understanding that insurance
companies, not the doctor, make the decisions about what tests I can have and
what drugs I can take. Most tests are only allowed when there are symptoms --
unless it is an approved age-related screening like a colonoscopy or a
mammogram. Once you have been diagnosed with cancer it seems to me screenings
for metastases should be mandatory, but they are not. That may be because of
the desire to limit radiation exposure, or perhaps there just isn't enough
money available from the insurance company to pay for additional diagnostics.
Since my disease, the HER 2 neu kind, tends to metastasize to the brain more
often than other types, it seems only logical to have brain scans at least
yearly whether or not there are symptoms. Treating a small tumor usually has a
more favorable outcome for length of survival than does treating a large or
numerous tumors. But, no, finding cancer when it is small is not the goal, so
no brain scan for me right now. Sure, I could make up some symptoms, but I
don't want to do that.
After three hours of mostly waiting for my blood tests, CT scan,
MUGA scan, and next infusion to be scheduled, I finally felt that I had
accomplished the goal of changing treatments to a facility closer to home.
On Friday that all changed. The nurse from the new oncologist's
office called and said, "Your insurance is terminating on August 1st. If
your insurance is to continue under the same plan or if you change insurance
companies, we will need your deductible paid in full prior to any
treatments." Our insurance is being renewed -- thankfully -- but and it is
a big BUT, our deductible is $10,000! Nope, that amount of money doesn't exist
in any of my bank accounts right now. The hospital in Chapel Hill has never
asked for a lump sum payment of our deductible. Instead, they set-up a payment
plan which is allowing us to manage the huge amount of debt we incur each year
I live. The final words the woman said to me before ending our phone call
haunts me still. I said to her, "I guess I will have to continue
treatments in Chapel Hill." She said, ". . . if they will take you
back." Good grief, I am at the mercy of so many people.
Today is Tuesday, one week and one day after my infusion. I spoke
with the nurse navigator in Chapel Hill yesterday, and my treatments can
continue as usual. It is disappointing after the many weeks it has taken to try
to be treated closer to home to have it all fall apart because of our inability
to pay for the switch. At least, the up-side is my daughter will be attending
UNC-Chapel Hill in the fall which means I will be able to see her every time I
have an appointment. I am happy about that.
Next appointment, scans will be reviewed. NERVOUS